Lisa Maier
Drug-Microbiome-Interactions
University of Tübingen
Faculty in: IMPRS
Vita

- PhD, ETH Zurich, 2010 - 2014
- Postdoc, EMBL Heidelberg, 2015 - 2018
- Junior Group Leader, University of Tübingen, 2019 – 2022
- Professor for Microbiome-Host-Interactions, University of Tübingen, from 2022
Research Interest
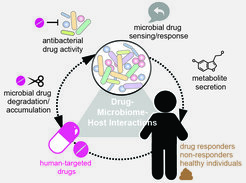
Drug-Microbiome-Host Interactions
Medication has arisen as one of the most impactful factors on the gut microbiota composition and we identified a generalized effect of non-antibiotics on gut microbes (24% of the tested FDA-approved human-targeted drugs). For the vast majority of these drug-microbe interactions, we do not know the underlying drug targets in microbes and do not understand whether they have beneficial (required for the drug to work) or detrimental (side) effects for humans. In our lab, we want to further investigate questions at the drug-microbiome-host interface. Specifically, we aim at understanding how drugs can impact communities and whether one could use drugs to restore a healthy balance.
Microbial Colonization Dynamics
In the healthy gut, the microbiota generally provides “colonization resistance”, prohibiting the intrusion of new microbes into the community and protecting the host from enteropathogen infection. However, antibiotic-mediated microbiota perturbations disrupt this protective shield, resulting in infection, in particular with broadly antibiotic-resistant nosocomial pathogens such as vancomycin-resistant Enterococcus faecium, Gram-negative Enterobacteriaceae and Clostridium difficile. Additionally, not only antibiotic therapy but also many other factors, such as certain diseases or dietary changes, can promote intestinal colonization with intruders. We want to understand the mechanisms underlying their colonization and long-term persistence in the community.
Microbiome Modulation
We aim at harnessing our understanding of drug-microbe and pathogen-commensal interactions in order to modulate the microbiome towards a balanced microbial community that prevents pathogen invasion and silences indigenous opportunistic pathogens (often referred to as pathobionts). Such microbiome modulation can be achieved by drugs with defined spectrum activity against specific microbes or microbial consortia. Alternatively, antagonistic drug interactions can be used to direct the spectrum of activity to a specific (sub-) group of bacteria. Since the microbiome composition is individual specific, so would be, at least to some degree, the solutions. Thus, the ultimate goal will be precision medicine strategies that will help to alleviate and cure microbiome-associated diseases.
Available PhD Projects
- Currently not recruiting PhD students via the IMPRS
Selected Reading
- De la Cuesta-Zuluaga, J., Müller, P., Maier, L. (2024). Balancing Act: Counteracting Adverse Drug Effects on the Microbiome. Trends Microbiol. DOI: 10.1016/j.tim.2024.09.011
- de la Cuesta-Zuluaga, J., Boldt, L., Maier, L. (2024). Response, resistance, and recovery of gut bacteria to human-targeted drug exposure. Cell Host Microbe, 32(6):786-793. https://doi.org/10.1016/j.chom.2024.05.009
- Müller, P. #, de la Cuesta-Zuluaga, J. #, Kuhn, M., Baghai Arassi, M., Treis, T., Blasche, S., Zimmermann, M., Bork, P., Patil, K.R, Typas, A., Garcia-Santamarina, S.*, Maier, L. *(2024) High-Throughput Screening Strategies for Identifying Compounds Acting against Gut Bacteria. Nat. Protoc, Mar;19(3):668-699,https://doi.org/10.1038/s41596-023-00926-4
- Maier, L. #*, Goemans, C. V#., Wirbel, J., Kuhn, M., Eberl, C., Pruteanu, M., Müller, P., Garcia-Santamarina, S., Cacace, E., Zhang, B., Gekeler, C., Banerjee, T., Anderson, E. E., Milanese, A., Löber, U., Forslund, S. K., Patil, K. R., Zimmermann, M., Stecher, B., Zeller, G., Bork, P., & Typas, A.*(2021) Unravelling the collateral damage of antibiotics on gut bacteria. Nature, 599, pages 120–124, https://doi.org/10.1038/s41586-021-03986-2
- Maier, L.#, Pruteanu, M.#, Kuhn, M. #, Zeller, G., Telzerow, A., Anderson, E. E., Brochado, A. R., Fernandez, K. C., Dose, H., Mori, H., Patil, K. R., Bork, P., & Typas, A. (2018). Extensive impact of non-antibiotic drugs on human gut bacteria. Nature, 555(7698), 623-628. https://doi.org/10.1038/nature25979

